Stem cells restore sight in rabbits and humans
In two different studies, stem cells have been used to regenerate parts of the eye and restore sight to both blind rabbits and blind humans.
We've really only just begun to probe the potential of stem cells and the implications they will have on human health, but new research from two separate international teams shows that their potential as a cure for blindness is outstanding.
The two teams each used adult stem cells to regenerate parts of the eye and restore sight to the blind.
One team, from Cardiff University in the UK and Osaka University in Japan, grew a variety of cells, using one particular type to cure induced blindness in lab rabbits.
The second team, from the University of California, San Diego School of Medicine and Shiley Eye Institute alongside colleagues in China, generated human lens cells, using them to restore sight to human infants with congenital cataracts. Both studies were published this week in the journal Nature.
The team from Cardiff and Osaka (paper) used induced pluripotent stem cells. These are stem cells that can be harvested from a human and reverse-engineered back to a state from which they can develop into a number of different cells.
The eye is complex, and its cells highly specialised. While lens and cornea cells have been developed from stem cells previously, this new study was able to develop lens, cornea and conjunctiva. The viability of the corneal epithelial cells was put to the test on rabbits that had been blinded for the purpose of this research.
"This research shows that various types of human stem cells are able to take on the characteristics of the cornea, lens and retina," said study co-author Andrew Quantock of Cardiff University in a statement.
"Importantly, it demonstrates that one cell type -- the corneal epithelium -- could be further grown in the lab and then transplanted on to a rabbit's eye where it was functional, achieving recovered vision."
The UCSD team only focused on one type of cell, but they used it to cure blindness in humans (paper). They used endogenous stem cells. Rather than having to implant pluripotent stem cells into the site, endogenous stem cells are stem cells that are already in place. Lens epithelial stem cells, or LECs, are cells that will regenerate lens cells over the course of a person's life.
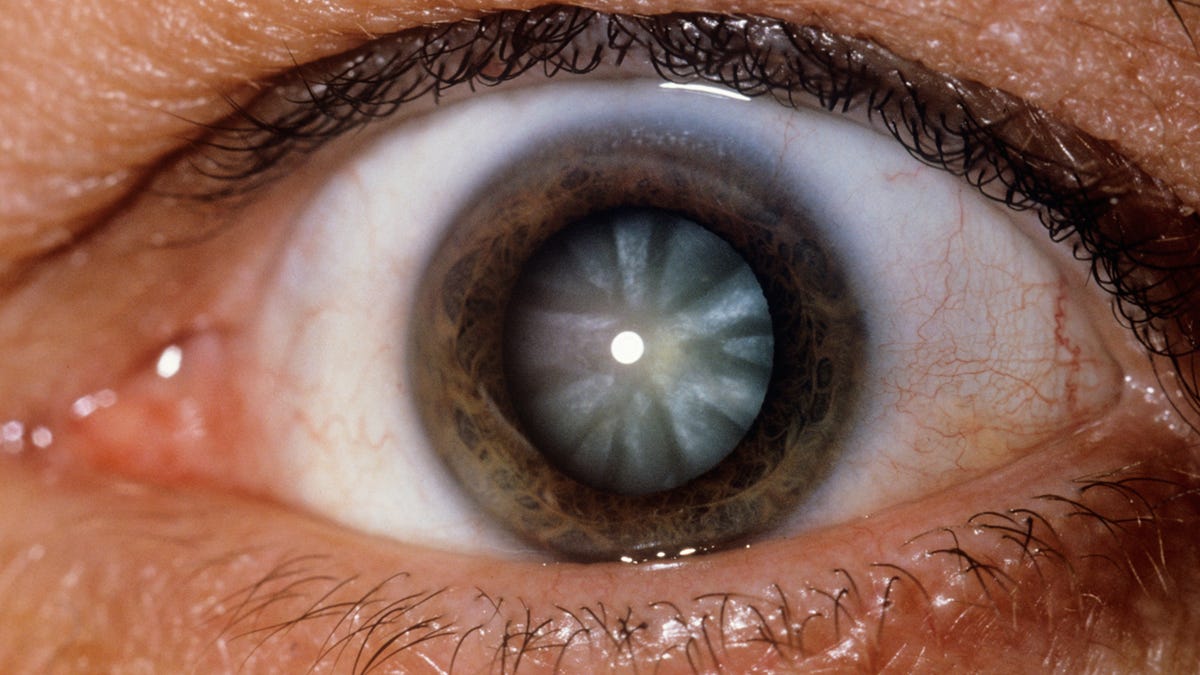
The study involved infants born with cataracts. These are usually corrected with surgery, which involves the removal of the cataract and the implantation of an artificial lens.
The team employed a new, minimally invasive surgical technique designed to make use of the LECs present in the patient's eye. It preserves the lens capsule, which gives the lens its shape, and stimulates the LECs.
They operated on 12 infants under the age of two years, removing the cataracts from their eyes and leaving the LECs intact. These were compared to a control group of 25 infants who had undergone the standard procedure.
The control group experienced higher rates of post-surgery inflammation, early-onset ocular hypertension and lens clouding. The 12 infants who underwent the new procedure healed much faster, and, after three months, every patient had regenerated clear, bioconvex lenses.
Using the patient's own tissue helps reduce the risk of immune rejection and the transmission of pathogens that could occur with the use of foreign tissue.
"The success of this work represents a new approach in how new human tissue or organ can be regenerated and human disease can be treated, and may have a broad impact on regenerative therapies by harnessing the regenerative power of our own body," said study leader Kang Zhang of the UCSD School of Medicine in a statement.